Diabetes, a chronic metabolic disorder characterized by elevated blood glucose levels, is a significant health concern globally. In the context of men’s health, understanding the nuances of diabetes in men is paramount given its prevalence and potential complications. Type 2 diabetes, formerly known as adult-onset diabetes, is the most prevalent type of diabetes, affecting a significant majority—around 90% to 95%—of the 13 million men diagnosed with the condition. The prevalence of diabetes has seen a notable surge across all states, with men experiencing one of the most significant increases.Typically, the risk of developing type 2 diabetes escalates with age. The American Diabetes Association suggests that individuals without other risk factors should begin screening for the condition after reaching the age of 45.
Types of Diabetes in Men
- Type 1 diabetes, often diagnosed in childhood or early adulthood, results from the body’s inability to produce insulin. This autoimmune condition requires lifelong insulin therapy and careful monitoring to prevent complications. Symptoms such as excessive thirst, frequent urination, and unexplained weight loss may prompt diagnosis.
- Type 2 diabetes, the most common form, typically develops later in life and is often associated with obesity and sedentary lifestyles. Insulin resistance and impaired insulin secretion contribute to its pathogenesis. Symptoms may be subtle initially, but over time, individuals may experience fatigue, blurred vision, and slow wound healing.
- Gestational diabetes, though predominantly affecting pregnant women, can also occur in men, albeit rarely. It poses risks to both the father’s and offspring’s health, necessitating careful monitoring and management during pregnancy.
Typically, the risk of developing type 2 diabetes escalates with age. The American Diabetes Association suggests that individuals without other risk factors should begin screening for the condition after reaching the age of 45.
In contrast to type 1 diabetes, where the body produces little to no insulin, individuals with type 2 diabetes do produce insulin, but it’s either insufficient or not effectively utilized—a phenomenon referred to as insulin resistance.
When there’s an insulin deficiency or it’s not utilized properly, glucose, or sugar, cannot enter cells for energy production. Consequently, sugar accumulates in the bloodstream, impairing cellular function. This buildup of sugar can lead to several issues, including:
- Dehydration: Excess sugar in the blood prompts frequent urination, causing significant fluid loss and subsequent dehydration.
- Hyperosmolar nonketotic diabetic coma: In severe cases of dehydration, where fluid intake doesn’t compensate for losses, individuals may experience this dangerous complication.
- Body damage: Prolonged elevation of blood sugar levels can harm nerves and small blood vessels, increasing the risk of complications such as diabetic retinopathy, nephropathy, and cardiovascular diseases like atherosclerosis, which can culminate in heart attacks or strokes.
Who is Prone to Type 2 Diabetes?
Type 2 diabetes doesn’t discriminate—it can affect anyone. However, certain groups are at a higher risk, including individuals who:
- Are overweight or obese
- Have family members with a history of type 2 diabetes.
- Experience metabolic syndrome, characterized by a combination of issues like high cholesterol, triglycerides, low levels of HDL (“good”) cholesterol, high LDL (“bad”) cholesterol, and high blood pressure.
- Lead sedentary lifestyles, lacking physical activity.
- Consume diets rich in sugar and refined carbs while lacking fiber and whole grains.
- Belong to certain ethnic groups such as African American, Hispanic, American Indian, Alaska Native, Pacific Islanders, or some Asian American communities.
- Additionally, advancing age increases susceptibility to the disease, as aging reduces the body’s tolerance to sugars.
What Triggers Type 2 Diabetes?
While more prevalent than type 1 diabetes, the precise causes of type 2 diabetes remain somewhat elusive, likely stemming from a combination of factors rather than a singular issue.
Type 2 diabetes often has a familial tendency, but the exact mode of inheritance or the specific genetic factors contributing to it remains unclear.
What are the Signs of Type 2 Diabetes?
Symptoms of type 2 diabetes can vary among individuals but may include:
- Increased thirst.
- Heightened hunger, particularly after meals.
- Dry mouth.
- Nausea and occasional vomiting.
- Frequent urination.
- Persistent fatigue, feeling weak or tired.
- Blurred vision.
- Numbness or tingling sensations in the hands or feet.
- Recurrent skin or urinary tract infections.
- In rare cases, diagnosis may occur after displaying symptoms while in a diabetic coma in a hospital setting.
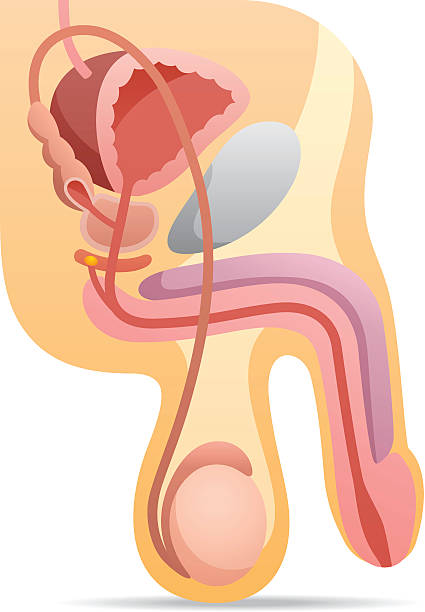
Health Implications of Diabetes in Men
Diabetes substantially increases the risk of cardiovascular complications in men. Atherosclerosis, characterized by the buildup of plaque in the arteries, raises the likelihood of heart attacks and strokes. Additionally, hypertension, often exacerbated by diabetes, further elevates cardiovascular risks.
Sexual health issues, including erectile dysfunction and decreased libido, are prevalent among men with diabetes. Vascular and neurological factors contribute to these complications, impacting both physical and psychological well-being.
Neuropathy, a common consequence of diabetes, manifests as peripheral nerve damage, leading to sensations of tingling, numbness, and pain in the extremities. Foot complications, such as ulcers and infections, pose significant risks, potentially necessitating amputation in severe cases.
How is Type 2 Diabetes Identified?
If your healthcare provider suspects you have type 2 diabetes, they’ll first examine your blood for indicators like high sugar levels. Additionally, they may analyze your urine for the presence of sugar or ketone bodies.
Diagnostic tests commonly used for type 2 diabetes include the fasting plasma glucose test and the casual plasma glucose test.
Complications Associated with Type 2 Diabetes
When type 2 diabetes isn’t managed effectively, it can lead to severe or life-threatening complications, such as:
- Retinopathy: People with type 2 diabetes may already experience eye issues linked to the condition. Over time, even individuals without preexisting eye problems related to diabetes may develop some form of eye ailment. Controlling not just sugar levels but also blood pressure and cholesterol is crucial to prevent worsening eye diseases. Fortunately, most cases do not result in significant vision loss.
- Kidney damage: The risk of kidney disease escalates with the duration of diabetes. Prolonged diabetes significantly increases the risk of serious conditions like kidney failure and heart disease.
- Impaired blood circulation and nerve damage: Nerve damage and arterial hardening reduce sensation and blood flow in the feet, increasing the likelihood of infections and poorly healing ulcers. Consequently, there’s a heightened risk of amputation. Nerve damage may also manifest as digestive issues like nausea, vomiting, and diarrhea.
How Can Diabetes Be Prevented?
Plenty can be done to prevent type 2 diabetes. Studies indicate that a whopping 90% of cases could be prevented or substantially delayed by adopting a healthier lifestyle, including dietary improvements and adequate physical activity.
A pivotal study involving 3,234 overweight individuals with elevated blood glucose levels, putting them at high risk of diabetes, demonstrated remarkable results. Those who adhered to a program combining exercise and diet aimed at shedding excess weight—an average of 15 pounds—lowered their diabetes risk by 58%. Among participants aged 60 and older, the risk reduction was even more substantial, at 71%. Remarkably, these individuals were already predisposed to diabetes.
Experts emphasize maintaining a healthy weight and staying physically active as key strategies to significantly reduce the likelihood of developing diabetes.
How is Diabetes Managed?
Receiving a diabetes diagnosis doesn’t signify the end of the road. In many instances, lifestyle adjustments alone can effectively manage the condition. However, numerous individuals with diabetes may require oral or injectable medications to regulate blood sugar levels.
When these measures prove insufficient, insulin—administered via inhalation or injection—might become necessary, sometimes complemented by oral medications. The FDA has sanctioned several innovative drugs that collaborate with insulin to enhance blood sugar control.
Although treatment options have advanced, managing diabetes remains challenging, prompting a continued emphasis on prevention by healthcare experts.
Management and Treatment Options
Lifestyle modifications form the cornerstone of diabetes management in men. Emphasizing balanced nutrition, low glycemic index foods, and regular physical activity can improve blood glucose control and mitigate complications.
Medication and insulin therapy play vital roles in managing diabetes, particularly in Type 2 diabetes where oral medications or injectable insulin may be necessary to achieve glycemic targets.
Regular monitoring of blood glucose levels, coupled with comprehensive annual evaluations, allows for early detection of complications and adjustments to treatment plans.
Psychological and Emotional Impact
Living with diabetes can induce significant psychological distress in men. Stress, anxiety, and depression are common, necessitating holistic approaches to diabetes care that address mental health needs. Coping strategies, such as mindfulness techniques and peer support groups, can alleviate emotional burdens and enhance overall well-being.
What Else Should I Know About Diabetes?
Experts advise adopting a healthy diet to thwart the onset of type 2 diabetes, which includes incorporating whole grains, fruits, and vegetables while limiting sugar and refined carbohydrates.
Interestingly, research suggests that moderate alcohol consumption might confer protection against diabetes. A synthesis of data from 15 studies revealed that moderate drinking slashed the risk of type 2 diabetes by nearly 30%. However, excessive alcohol intake was associated with heightened risk. As always, moderation is key—such as limiting alcohol consumption to one drink per day.
sources:
- National Diabetes Information Clearinghouse: “Essential Knowledge on Type 2 Diabetes.”
- Intellihealth: “Understanding Type 2 Diabetes.”
- UpToDate: “Overview of Type 2 Diabetes for Patients (Extended Insights).”
- American Heart Association: [No specific title provided].
- Diabetes Care: “Reduced Type 2 Diabetes Risk Linked to Moderate Alcohol Intake: Analysis of Prospective Observational Studies.”
- David Ludwig, MD, PhD, Associate Professor of Pediatrics at Children’s Hospital, Boston.
- Journal of the American Medical Association: “Association Between Sugar-Sweetened Beverages, Weight Gain, and Type 2 Diabetes Incidence in Young and Middle-Aged Women.”