The male reproductive system is responsible for sexual function and the creation of offspring in individuals designated male at birth. It consists of both internal and external organs that work together to produce, store, and release sperm, which is needed for fertilizing eggs and initiating pregnancy within the female reproductive system. Additionally, this system produces vital hormones like testosterone, crucial for male development.
However, these organs don’t fully activate until puberty, a phase marking the transition from childhood to adulthood. Puberty begins when the hypothalamus and pituitary gland release hormones signaling the testicles to produce testosterone and sperm. Testosterone, the primary male sex hormone, drives the growth and maturation of the penis, testicles, and scrotum, as well as structures like the prostate gland and seminal vesicles, essential for semen production. Moreover, testosterone influences secondary sexual characteristics, which include:
- Growth of hair in the genital area, face, and armpits
- Development of muscles
- Deepening of the voice and other vocal changes
- Height increase due to growth spurts
Male Reproductive System Functions
The primary functions of the male reproductive system revolve around the production and delivery of sperm, which is essential for fertilization. These functions include:
- Production of spermatozoa (sperm cells) through a process called spermatogenesis.
- Secretion of male sex hormones, particularly testosterone, which regulates secondary sexual characteristics and maintains reproductive function.
- Transporting sperm from the testes through a series of ducts to mix with seminal fluids, forming semen.
- Delivering semen through the urethra during ejaculation for potential fertilization of a female egg.
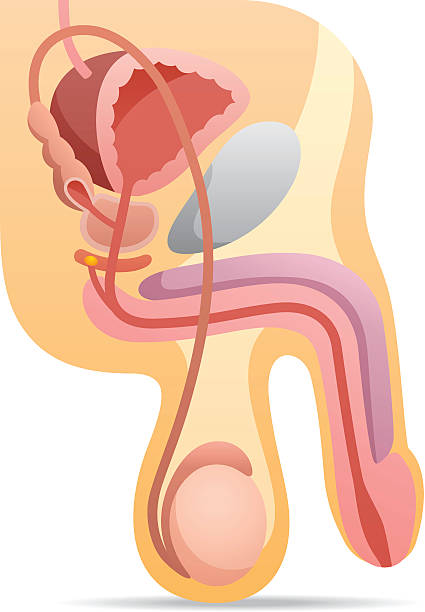
Parts and Functions of the Male Reproductive System
The male reproductive system mainly consists of external structures, unlike the female reproductive system.
The external organs of the Male reproductive system
These include the following:
- Penis: This is the male organ involved in sexual intercourse. It consists of three parts: the root, which connects to the abdominal wall; the body or shaft; and the glans, which is the cone-shaped tip. The glans are covered by a loose layer of skin called the foreskin, which may be removed through circumcision. The urethral opening, through which both semen and urine pass, is located at the tip of the penis. The glans contain sensitive nerve endings. The body of the penis is cylindrical and consists of three spongy chambers that fill with blood during sexual arousal, causing the penis to become erect. The skin of the penis is elastic, allowing for changes in size during erection. Semen, containing sperm, is ejaculated through the end of the penis during orgasm. When erect, the urethra’s flow of urine is blocked to allow only semen to be expelled.
- Scrotum: This is a loose, pouch-like sac of skin located behind and below the penis. It houses the testicles and contains numerous nerves and blood vessels. The scrotum acts as a climate control system for the testes, regulating their temperature slightly cooler than the body’s temperature, crucial for sperm development. Special muscles in the scrotum’s wall contract and relax to adjust the testicles’ proximity to the body for temperature regulation.
- Testicles (Testes): These are oval-shaped organs about the size of large olives, situated within the scrotum. Most individuals have two testes. The testes produce testosterone, the primary male sex hormone, as well as other hormones like inhibin B, insulin-like factor 3, Mullerian inhibiting substance hormone (or anti-Mullerian hormone), and estradiol. They also produce sperm through coiled tubes called seminiferous tubules.
- Epididymis: This is a long, coiled tube located behind each testicle. It transports and stores sperm produced in the testes. Additionally, the epididymis facilitates the maturation of sperm, as sperm emerging from the testes are initially immature and incapable of fertilization. During sexual arousal, contractions propel sperm into the vas deferens.
Also note that these external structures play vital roles in the male reproductive system, facilitating sexual function, sperm production, and fertilization.
The internal organs of the male reproductive system:
These are known as accessory organs. Here’s a breakdown of these internal structures:
- Vas Deferens: This is a lengthy, muscular tube that extends from the epididymis into the pelvic cavity, situated just behind the bladder. Its primary function is to carry mature sperm to the urethra in preparation for ejaculation.
- Ejaculatory Ducts: Formed by the fusion of the vas deferens and seminal vesicles, these ducts empty into the urethra. They play a key role in transporting seminal fluid during ejaculation.
- Urethra: The urethra serves as a passage for both urine and semen. During sexual arousal, the flow of urine is blocked, allowing only semen to be ejaculated at orgasm.
- Seminal Vesicles: These sac-like pouches attach to the vas deferens near the base of the bladder. They produce a fluid rich in fructose, which provides energy for sperm motility. The seminal fluid from the vesicles constitutes the majority of ejaculatory fluid.
- Prostate Gland: Positioned below the bladder and in front of the rectum, the prostate gland is roughly the size of a walnut. It secretes additional fluid into the ejaculate, aiding in sperm nourishment. The urethra passes through the center of the prostate gland. Moreover, the prostate converts some testosterone into dihydrotestosterone (DHT), which influences sexual development and certain adult functions such as prostate growth and male pattern baldness.
- Bulbourethral Glands (Cowper’s Glands): These pea-sized glands are located alongside the urethra just below the prostate gland. They produce a clear, lubricating fluid that is released directly into the urethra, aiding in lubrication and neutralizing any acidity from residual urine.
The internal organs of the male reproductive system, known as accessory organs, play crucial roles in sperm transport, semen production, and ejaculation. Below is a breakdown of these internal structures:
Together, these internal organs play essential roles in sperm transport, semen production, and the process of ejaculation, ensuring the reproductive system functions properly.
Male Reproductive Hormones
The male reproductive system is regulated by several hormones, including:
- The male reproductive system relies heavily on hormones, which act as chemical messengers controlling various cellular and organ activities. There are two main types of hormones crucial for sexual function and characteristics:
- Androgens: These are predominantly found in higher levels in individuals assigned male at birth (AMAB). Testosterone is the most well-known androgen. It plays a vital role in sperm production and is responsible for developing male traits such as muscle mass, bone density, facial hair growth, deepening of the voice, and libido.
- Estrogens: While estrogen levels are typically higher in individuals assigned female at birth (AFAB), men also have small amounts of estrogen. Estrogen is important for female growth and reproductive development. In men, low estrogen levels can lead to reduced sexual interest and increased abdominal fat, while high estrogen levels may result in infertility, breast enlargement, and erectile issues.
In addition to testosterone, two other key hormones in the male reproductive system are follicle-stimulating hormone (FSH) and luteinizing hormone (LH). These hormones are produced by the pituitary gland, a small gland located at the base of the brain.
- Follicle-Stimulating Hormone (FSH): FSH is essential for spermatogenesis, the process of sperm production.
- Luteinizing Hormone (LH): LH stimulates the production of testosterone, which is necessary for sperm production.
These hormones work in coordination to regulate the various functions of the male reproductive system, including sperm production and the development of secondary sexual characteristics.
Male Reproductive System Diseases
The male reproductive system is susceptible to various disorders and conditions, including:
- Erectile Dysfunction: This condition involves difficulty in achieving or maintaining an erection, alongside a decreased desire for sexual activity.
- Premature Ejaculation: Characterized by ejaculation occurring earlier than desired, often before or shortly after penetration.
- Phimosis: When the foreskin cannot be retracted, leading to symptoms like redness, swelling, soreness, and discomfort during urination or sex.
- Paraphimosis: This condition results in the foreskin becoming trapped behind the head of the penis, posing a risk of cutting off circulation and causing symptoms such as pain, swelling, and discoloration.
- Epididymitis: Inflammation of the epididymis, manifesting as swelling, pain, or tenderness in the scrotum or testicles, painful urination, discharge, and discomfort in the pelvic area.
- Male Infertility: The inability to impregnate a partner despite regular, unprotected intercourse for at least a year.
- Peyronie’s Disease: This condition leads to curvature or bending of the penis, accompanied by hard lumps, pain during erection or intercourse, and alterations in penis shape.
- Sexually Transmitted Infections (STIs): Symptoms vary depending on the specific infection but can include genital sores, discharge, swelling, itching, and pain during sex or urination.
- Low Testosterone (Hypogonadism): Signs of low testosterone include decreased libido, fatigue, muscle loss, irritability, erectile dysfunction, and depression.
- Priapism: Persistent erection unrelated to sexual arousal, often accompanied by pain, penile rigidity, and worsening discomfort over time.
- Testicular Torsion: A medical emergency causing severe testicular pain, swelling, a visible lump, discoloration of the scrotum, nausea, vomiting, and fever due to restricted blood flow to the testicles.
- Varicocele: Enlarged veins in the scrotum leading to dull pain, swelling, testicular shrinkage, and a small lump, potentially affecting fertility.
- Hypospadias: A congenital condition where the urethra opens on the underside of the penis, resulting in a curved appearance, incomplete foreskin coverage, and abnormal urine flow.
- Testicular Cancer: Symptoms include testicular lumps or swelling, a heavy sensation in the scrotum, abdominal or groin pain, breast enlargement or tenderness, back pain, and sudden scrotal swelling.
- Penile Cancer: Manifestations comprise thickened or discolored penile skin, penile lumps, bleeding sores, rash, crusty bumps, swelling, foul-smelling discharge, and changes in foreskin appearance.
- Prostate Cancer: Symptoms typically arise in advanced stages and may include urinary difficulties, blood in urine or semen, erectile dysfunction, bone pain, weakness or numbness in legs or feet, incontinence, weight loss, and fatigue.
Tips for Maintaining a Healthy Reproductive System
Maintaining a healthy reproductive system throughout your life is crucial, and there are several proactive steps you can take to achieve this:
- Regular STI Testing: It’s essential to get a sexually transmitted infection (STI) test according to your sexual activity. The Centers for Disease Control and Prevention (CDC) recommends at least one HIV test for everyone between the ages of 13 and 64. If you’re sexually active, especially if you have multiple partners, annual testing for chlamydia, gonorrhea, syphilis, and HIV is advised. Those engaging in higher-risk behaviors should consider more frequent HIV testing, and discussing testing with a doctor is important for those engaging in oral or anal sex.
- Practicing Good Hygiene: Keeping the genital area clean is crucial for preventing infections. For uncircumcised individuals, it’s essential to pull back the foreskin and thoroughly clean and dry the penis head.
- Practicing Safe Sex: Consistently using condoms during sexual activity can significantly reduce the risk of STIs.
- Managing Chronic Health Conditions: Managing chronic health conditions is crucial for overall well-being, especially concerning issues like erectile dysfunction. Several diseases can exacerbate this condition due to their impact on blood flow and other factors. Some of these conditions include:
- Type 2 Diabetes: Diabetes can affect blood vessels and nerves, impairing the ability to achieve or maintain an erection.
- High Blood Pressure (Hypertension): Elevated blood pressure can damage blood vessels, reducing blood flow to the penis and hindering erectile function.
- Heart Disease: Conditions like coronary artery disease can lead to restricted blood flow, affecting erectile function as well.
- High Cholesterol: High levels of cholesterol can lead to the buildup of plaque in arteries, impeding blood flow and potentially causing erectile difficulties.
- Obesity: Excess weight can contribute to various health problems, including diabetes and heart disease, which in turn can impact erectile function.
- Getting the HPV Vaccine: Protecting against human papillomavirus (HPV) through vaccination can prevent various cancers and genital warts. Physicians vaccine recommend HPV vaccine for individuals aged 9 to 45.
- Avoiding Smoking: Smoking not only increases the risk of cancer and heart disease but also contributes to erectile dysfunction.
- Performing Self-Checks: Regular self-examinations can help detect any unusual changes in the penis, testicles, and scrotum, such as lumps or swelling. Feeling each testicle is important for detecting abnormalities.
- Discussing Prostate Cancer Screening: Talk to your doctor about whether prostate cancer screening is appropriate for you. This decision should be made considering the risks and benefits, with guidance from your healthcare provider.
- Consider Circumcision: Circumcision can reduce the risk of urinary tract infections, STIs, and penile cancer. It also eliminates the risk of conditions like phimosis and paraphimosis.
- Maintaining a Healthy Weight: health professionals link Obesity to erectile dysfunction, so maintaining a healthy weight can improve erectile function. Losing weight can positively impact your ability to achieve and maintain erections.
However, adopting these proactive measures, you can support the health and functionality of your reproductive system throughout your life.
Keynote
The male reproductive system is a complex network of organs, hormones, and physiological processes essential for fertility and sexual function. Understanding its anatomy, functions, and potential health issues is crucial for maintaining reproductive health and overall well-being.
Frequently asked questions
Curious about how the male reproductive system works? Let’s dive into some common questions:
1. What’s the role of testosterone in the male reproductive system?
Testosterone is like the engine driving the male reproductive system. It’s essential for developing male reproductive organs, producing sperm, and shaping manly traits like facial hair and a deep voice.
2. Any interesting facts about the male reproductive system?
Absolutely! Here are a few:
- While everyone born male has a male reproductive system, it doesn’t fully kick into gear until puberty, which typically starts more than 10 years after birth.
- Unlike the female reproductive system, a lot of the male parts are on the outside of the body.
- Beyond its sex role, testosterone also influences other things like body hair growth and even baldness.
In conclusion, the male reproductive system is intricate and vital for human reproduction and overall health. Also, understanding its components, functions, and potential issues, individuals can take proactive steps to maintain reproductive health and well-being
Sources:
- Merck Manuals: “Male Puberty.”
- Cleveland Clinic: “Understanding Testicular Function.”
- Cleveland Clinic: “Anatomy of the Male Reproductive System.”
- Cleveland Clinic: “Dihydrotestosterone (DHT).”
- Cleveland Clinic: “Role of Androgens in Male Health.”
- Endocrine Society: “Hormonal Regulation of Reproduction.”
- Merck Manuals: “Introduction to Pituitary Gland Function.”
- Mayo Clinic: “Understanding Erectile Dysfunction.”
- Cleveland Clinic: “Managing Premature Ejaculation.”
- Cleveland Clinic: “Treatment of Phimosis.”
- Cleveland Clinic: “Addressing Paraphimosis.”
- Mayo Clinic: “Overview of Epididymitis.”
- Johns Hopkins Medicine: “Factors Influencing Male Fertility.”
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): “Peyronie’s Disease.”
- Cleveland Clinic: “Prevention and Treatment of Sexually Transmitted Infections (STIs).”
- Urology Care Foundation: “Diagnosis and Management of Low Testosterone.”
- Mayo Clinic: “Understanding Priapism.”
- Cleveland Clinic: “Recognizing Testicular Torsion.”
- Cleveland Clinic: “Management of Varicocele.”
- Mayo Clinic: “Treatment Options for Hypospadias.”
- Mayo Clinic: “Comprehensive Guide to Testicular Cancer.”
- Urology Care Foundation: “Preventive Measures for Penile Cancer.”
- American Cancer Society: “Identifying Signs and Symptoms of Prostate Cancer.”
- CDC: “Guidance on STD Testing.”
- Cleveland Clinic: “Importance of HPV Vaccination.”
- Sexual Medicine Reviews: “Impact of Smoking on Erectile Function.”
- Mayo Clinic: “Step-by-Step Guide to Testicular Examination.”
- Mayo Clinic: “Recommendations for Prostate Cancer Screening.”
- Mayo Clinic: “Considerations Regarding Circumcision.”
- Obesity Action Coalition: “Exploring the Relationship Between Obesity and Sexual Function.”
- National Cancer Institute: “Study Reveals Gaps in Penile Cancer Treatment.”
- Nature Communications: “Understanding the Link Between Balding, Testosterone, and Skin Cancer.”