Do you experience severe jaw pain? It might be a sign of a condition called temporomandibular joint (TMJ) disorder. But don’t fret; there are ways to alleviate the discomfort right at home.
The TMJ, or temporomandibular joint, is the hinge that connects your jaw to your skull, allowing you to talk, chew, and yawn. Problems with this joint and the surrounding muscles are called TMJ disorders (TMDs).
Causes of TMJ Disorder
While the exact cause of TMDs remains unclear, several factors could contribute to its development. These include:
- Jaw injury from accidents or sudden impacts
- Teeth grinding or clenching, exerting excessive pressure on the joint
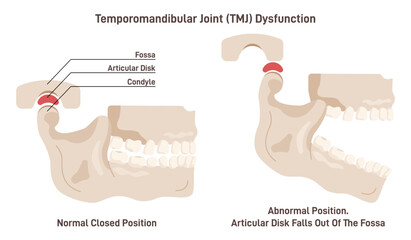
- Displacement of the cushioning disc between the joint’s ball and socket
- Arthritis affecting the joint
- Stress leading to muscle tightening or teeth clenching
Contrary to popular belief, TMDs aren’t typically caused by a misaligned bite or dental braces. Interestingly, women are more prone to TMDs compared to men, prompting researchers to explore differences in TMJ structure and mechanics between genders.
Symptoms of temporomandibular joint (TMJ) disorder
TMJ disorder often manifests with significant pain and discomfort, which can persist for varying durations. Symptoms may affect one or both sides of the face, with the condition being most prevalent among individuals aged 20 to 40. Common indicators include:
- Pain or tenderness in the face, jaw joint, neck, shoulders, and around the ears, especially during activities like chewing or speaking
- Difficulty opening the mouth wide
- Jaw stiffness or locking in open or closed positions
- Clicking, popping, or grinding noises in the jaw joint during movement
- Fatigue in the face muscles
- Challenges with chewing or an uncomfortable bite sensation
- Swelling on the face’s side
- Toothaches or earaches
- Hearing issues or ringing in the ears
- Headaches or migraines
- Dizziness
- Numbness or tingling sensations in the fingers
- Neck pain and discomfort in the upper shoulders
Recognizing these symptoms is crucial for prompt management and relief from TMJ disorder’s effects.
Diagnosing temporomandibular joint (TMJ) disorder
When you experience symptoms like jaw pain or difficulty chewing, it’s essential to determine the underlying cause. While TMJ disorder is a common culprit, other conditions such as tooth decay, sinus issues, arthritis, or gum disease can mimic its symptoms. To pinpoint the root cause, your dentist will conduct a thorough evaluation.
The Diagnostic Process:
- Health History and Physical Exam: Your dentist will begin by discussing your medical history and conducting a physical examination. They’ll assess your jaw joints for tenderness and listen for any unusual sounds, like clicks or pops, during movement. Additionally, they’ll evaluate the range of motion in your jaw and check for muscle abnormalities.
- Imaging Tests: To obtain a comprehensive view of your jaw structure, your dentist may recommend full-face X-rays. These images allow them to examine the jawbones, TMJs, and teeth for any abnormalities. In some cases, additional imaging tests, such as MRI or CT scans, may be necessary. An MRI helps visualize the positioning of the TMJ disc during jaw movement, while a CT scan provides detailed images of the joint’s bony structures.
- TMJ Arthroscopy: In certain situations, your doctor or dentist may suggest TMJ arthroscopy for a more precise diagnosis. This minimally invasive procedure involves inserting a small camera near the jaw joint to examine it closely and make an accurate assessment.
- Referral to Specialists: Depending on the severity of your condition, you may be referred to an oral surgeon or an orthodontist for further evaluation and treatment. Oral surgeons specialize in surgical procedures related to the face, mouth, and jaw, while orthodontists focus on aligning teeth and correcting bite issues.
Home Treatments for TMJ Disorder
While professional intervention is crucial for managing TMJ disorder, there are several self-care measures you can take to alleviate symptoms:
- Over-the-Counter Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can help reduce muscle pain and swelling associated with TMJ disorder.
- Moist Heat or Cold Packs: Apply an ice pack to the affected area for about 10 minutes, followed by a warm compress for 5 minutes. This alternating therapy can help relieve pain and promote muscle relaxation.
- Soft Diet: Stick to soft foods like yogurt, mashed potatoes, and soup to minimize jaw strain. Avoid hard, crunchy, or chewy foods that require excessive chewing.
- Avoid Extreme Jaw Movements: Limit activities that require wide jaw movements, such as yawning, chewing gum, or singing loudly.
- Maintain Good Posture: Practice proper posture to reduce strain on your neck and facial muscles. Avoid resting your chin on your hand or holding the phone between your shoulder and ear.
- Teeth Positioning: Keep your teeth slightly apart to alleviate pressure on the jaw. Placing your tongue between your teeth can help prevent clenching or grinding.
- Relaxation Techniques: Explore relaxation techniques like deep breathing or meditation to reduce jaw tension. Physical therapy or massage may also be beneficial.
- Behavioral Changes: Avoid habits like chewing on pens or using your teeth as tools, which can exacerbate TMJ symptoms.
- Sleep Position: Sleeping on your back or side instead of your stomach can alleviate TMJ discomfort during sleep.
By incorporating these home treatments into your routine and seeking professional guidance as needed, you can effectively manage TMJ disorder and improve your quality of life.
Treating temporomandibular joint (TMJ) disorder
If you’re grappling with TMJ disorder, exploring treatment options with your dentist is crucial. Here’s what they might suggest:
- Medications: Your dentist can prescribe higher doses of NSAIDs to alleviate pain and swelling associated with TMJ disorder. They may also recommend muscle relaxants to ease jaw tension caused by teeth grinding or clenching. Additionally, antianxiety medications might be prescribed to alleviate stress, which can exacerbate TMD symptoms. These medications can also help manage pain when taken in low doses.
- Splint or Night Guard: These custom-made plastic mouthpieces are designed to prevent teeth clenching or grinding. A night guard is worn during sleep to protect your teeth and alleviate pressure on the jaw joint. On the other hand, a splint is worn throughout the day to correct bite alignment and reduce the effects of teeth grinding.
- Dental Work: Your dentist may recommend dental procedures such as replacing missing teeth, crowns, bridges, or braces to address bite irregularities and balance the surfaces of your teeth.
Additional Treatments:
If the initial treatments don’t provide adequate relief, your dentist may propose alternative therapies, including:
- Transcutaneous Electrical Nerve Stimulation (TENS): This therapy involves using low-level electrical currents to relax the jaw joint and facial muscles, providing pain relief. TENS therapy can be administered at the dentist’s office or at home.
- Ultrasound: Applying deep heat to the jaw joint can alleviate soreness and improve mobility, offering relief from TMJ symptoms.
- Trigger-Point Injections: Pain medication or anesthesia is injected into tender facial muscles, known as trigger points, to alleviate discomfort and promote relaxation.
- Radio Wave Therapy: Radio waves are used to stimulate the jaw joint, increasing blood flow and reducing pain associated with TMJ disorder.
- Low-Level Laser Therapy: This treatment helps lower pain and inflammation while improving neck mobility and jaw movement, enabling you to open your mouth more comfortably.
By exploring these treatment options in consultation with your dentist, you can find relief from TMJ disorder and improve your overall oral health and well-being.
Surgical Options for TMJ Disorders
When conventional treatments fail to provide relief for TMJ disorders, surgery becomes a viable option. However, it’s essential to thoroughly consider this decision since surgical interventions are irreversible. Seeking multiple opinions from different dental professionals, including oral surgeons, orthodontists, otolaryngologists, and prosthodontists, is advisable.
Types of TMJ Surgery:
- Arthrocentesis: This procedure is suitable for individuals with minimal TMJ disorder history but experiencing jaw locking. It’s a minor surgery typically performed in the dentist’s office under general anesthesia. During arthrocentesis, needles are inserted into the joint to wash it out. Special tools may be used to remove damaged tissue or dislodge a stuck disc or joint.
- Arthroscopy: Arthroscopic surgery involves using a specialized tool called an arthroscope, equipped with a lens and light, to visualize the inside of the joint. Under general anesthesia, a small incision is made in front of the ear, and the arthroscope is inserted to examine the joint. Inflammation may be removed, or the disc and joint realigned. This minimally invasive procedure results in smaller scars, fewer complications, and a shorter recovery period compared to open-joint surgery.
- Open-Joint Surgery: When arthroscopy is not feasible, open-joint surgery may be necessary. This type of surgery is indicated for conditions such as severe joint degeneration, tumors, or extensive scarring. Under general anesthesia, the entire area around the joint is opened up to provide better access and visibility. Open-joint surgery requires a longer recovery time and carries a higher risk of scarring and nerve injury compared to arthroscopic procedures.
- Modified condylotomy: This surgical approach targets the lower jaw (mandible) rather than the joint itself. It aims to alleviate pain and jaw locking by addressing issues related to the mandible.
Before opting for surgery, it’s crucial to discuss the potential risks, benefits, and expected outcomes with your dental care team. Additionally, thorough pre-surgical evaluations and consultations will help determine the most appropriate surgical approach based on your individual condition and needs.
Sources:
- American Academy of Otolaryngology—Head and Neck Surgery.
- National Institutes of Health (NIH): “TMD (Temporomandibular Disorders).”
- Cleveland Clinic: “Temporomandibular Joint (TMJ) Disorders.”
- Johns Hopkins: “Temporomandibular Disorder (TMD).”
- Mayo Clinic: “TMJ Disorders.”